Natural Born Killers
By Joseph Greenberg
 Every day the human body produces approximately 5,000 cancer cells
Every day the human body produces approximately 5,000 cancer cells
Cancer cells exist in all of our bodies. Thanks to the presence of Natural Killer (NK) cells that diligently patrol our system, these cells are prevented from mutating into dangerous cancerous growth. In light of this understanding, the world’s cancer researchers have tried to increase the number of NK cells in cancer sufferers as a way of treating those afflicted by the disease. Their efforts have been impressive but have ultimately yielded only mistakes and false hope. However, two Japanese doctors have innovated what they term an Amplified Natural Killer (ANK) therapy that can effectively treat cancer patients and limit the growth of cancerous tumours.
Aware of the aging population, the Japanese government passed, in April this year, the Cancer Prevention Act. The goal of the legislation is that the the cancer death rate be reduced by 20% among under 75-year olds within 10 years. According to a report about the legislation published in the Yomiuri newspaper, although there has been some decline in recent years, at present, approximately 320,000 Japanese die every year due to cancer. Globally, according to the World Health Organization (WHO), in 2005, roughly 13% of a total of 58 million deaths were the result of cancer. The WHO expects the number of cancer deaths to rise to an estimated 11.4 million by the year 2030.
The government of Japan hopes to meet the new law by increased efforts to combat smoking, introduction of more regular health checks and opening more cancer focused health consultation centers. While these efforts are welcomed by the medical community there is also an ongoing need for pharmaceutical and medical research and development. Japan’s history of cancer research developed significantly in the aftermath of the nuclear devastation of Hiroshima and Nagasaki. Although it can hardly be hailed as a silver lining, research on victims’ bones did lead to a major advancement by Japanese doctors in developing bone marrow transplants for cancer sufferers. While there are a number of treatments available for cancer, it shows little sign of fading into a problem of the past and for cancer sufferers, the treatments and therapies that they undergo often involve serious risks and dangerous side effects.
Currently, there are essentially three main types of treatment for cancer available:
Surgical oncology: the surgical removal of cancerous tumours
Radiotherapy: radio waves such as Xrays are used to lethally damage cancerous cells
Chemotherapy: treatment that includes the use of anti-cancer drugs that negatively affect mitosis (cell division) thus preventing the growth of a cancer.
Unfortunately, each of these therapies are problematic. The removal of cancerous tumours via surgery has limited effectiveness for a cancer that has spread all over the body. Radiotherapy is a powerful treatment but its strength is also its weakness. Radio waves can damage perfectly healthy cells, as well as having the potential to actually cause further cancerous mutation. Moreover, as not all cancer cells divide at the same time, a portion of cancer cells will always survive, thus requiring constant repetition of this dangerously potent therapy.
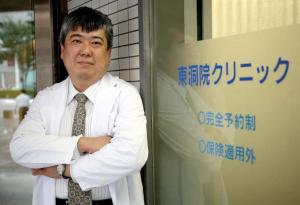 Dr Okubo of the Higashi-no-touin clinic in Kyoto -- Photography by David Coll Blanco
Dr Okubo of the Higashi-no-touin clinic in Kyoto -- Photography by David Coll Blanco
Chemotherapy is currently the most popular treatment but the problems are similar to those with radiotherapy— healthy cells can be damaged and once the cancer gets used to the drug, the cancer can resist it. There is also the risk of accelerated or new cancerous mutation.
In addition to the above therapies, immunotherapy—therapy that involves stimulating and manipulating the immune system—has also attracted a high degree of medical interest. It is in this field that two Japanese doctors—Dr Teshigawara and Dr Okubo—have innovated a new kind of therapy. Before detailing the nature of the therapy they have developed, it is perhaps worth going into the background of what cancer actually is and what cells the body has to fight it.
What is cancer?
In theory, cancer cells have been in existence for over 4 billion years. Before the evolutionary phase, roughly 530 million years ago, when animals evolved into hard-bodied entities—referred to as the Cambrian Explosion—the cells were in a state in which they divided and multiplied in a constant process, expanding and expanding. However, during this period, they evolved into regular cells constituting what eventually evolved into the human body. It was also with the Cambrian Explosion that cancer’s nemesis, NK cells, were brought into regular existence.
Every day, in the human body, an estimated 5,000 cancer cells are produced. What prevents the cells from actually developing into what we call a ‘cancer’—a group of expanding cancer cells that form a tumour—are the body’s NK cells, a part of the human immune system. Along with two other types of cell, NK cells are lymphocytes—a type of white blood cell. The three types of lymphocyte are as follows:
B-cells: developed in the bone marrow, B-cells become so-called plasma cells when they encounter an antigen and then release an anti-body that attaches itself specifically to that antigen. While B-cells are important in fighting infections, they play a relatively small role in preventing cancer.
T-cells: these cells pass through the blood stream at an early stage in their development and then grow stronger disease-fighting properties in the thymus gland near the heart. T-cells sometimes contain proteins that can identify cancerous cells and they rarely attack cancer cells, however, their most common function is to facilitate and regulate the activity of B-cells.
Natural Killer cells: less focused in what they attack, they respond to substances given off by cells involved in fighting diseased cells. When they find cancer cells, they are able to divide and destroy them before moving on to find more. They allow the cancer cells to multiply only to the level where a healthy balance is restored.
Thus, it is NK cells that are critical in making sure that we don’t all suffer from cancer. If we think of lymphocytes as an army, NK cells are the ones on the frontline. Dr Teshigawara and his partner Dr Okubo told us that it is probable that what we term ‘cancer’ is caused by an imbalance in the regular ratio of NK cells to cancer cells: when cancer cells have the upper hand, harmful cancerous growth takes place. With this in mind, an effective treatment is defined as a therapy that can successfully send the cancer into remission.
Immunotherapy
This kind of therapy essentially involves stimulation of the immune system to make it work in a more intelligent and efficient manner, or introducing elements from outside the body that fight diseases. For the first discovery and development of this technique, we should thank William B Coley, a New York physician trained at Harvard Medical School who in the late 1890s began to treat cancerous tumours by infecting patients with bacteria. While the treatment has many problems and patients often suffered greatly from the infection, modern medical science has made a number of improvements. Immunologists differentiate between two types of immunity: ‘acquired’ and ‘natural.’
 Dr Yuji Okubo (left) and Dr Keisuke Teshigawara
Dr Yuji Okubo (left) and Dr Keisuke Teshigawara
Acquired Immunity
Doctors have learned to help us acquire immunity from certain specific diseases; this is the basis of vaccines. Acquiring immunity often involves infecting people with a controlled version of a disease so that the body can learn to recognize the intruding cells and develop the antibodies to fight them. The problem with acquired immunity arises when outside entities develop a resistance to the antibodies.
Natural Immunity
This is our natural defense system against diseases—cells deal with outside entities, or the body’s own malfunctions without needing to be educated. The latter include the activities of NK cells in fighting cancer and also of cells such as macrophages that, among their other immune system roles, consume pathogens.
The majority of immunotherapy is focused on acquired immunity but there is a growing awareness of the potential of natural immunity, particularly when it comes to cancer. Sir Frank Macfarlane Burnet, who won the Nobel Prize for medicine in 1960, is looked upon by those in the field of immunology as a pioneer. It was Burnett who used the distinction between ‘self’ and ‘not self’ in his efforts to understand the human immune system and, it was also Burnet who came up with the theory of ‘immune surveillance’—referring to the part of the immune system that deals with self-generated errors and malfunctions.
In this sense, cancer is a ‘natural’ or ‘self’ problem—it does not come from outside the body—and NK cells are its ‘natural’ antithesis, focused on problems of the ‘self.’ It was this breakthrough that lead to the realization that NK cells have the best potential to effectively treat cancer. After years of study and trials, Teshigawara and Okubo, of the Higashi-no-touin clinic in Kyoto, have developed a therapy that can increase the number of NK cells: Amplified Natural Killer (ANK) therapy.
A new lymphocyte therapy
Previous lymphocyte treatments have been unable to increase the number of NK cells efficiently. One form of treatment involves removing lymphocytes from the blood and using a substance called IL-2 (a form of interleukin) to ‘activate’ the cells before returning them to the blood: Lymphokine Activated Killer (LAK) Therapy.
In the 1980s, Dr Steven A Rosenberg of the National Cancer Institute in Bethesda (US), developed a variety of LAK therapy using IL-2 to increase the number of NK cells. However, this treatment turned out to be less of a breakthrough than originally thought. Rosenberg was only able to increase the number of NK cells by 10—when increasing them more than this, the NK cells became less active and ineffective. In order to make up for the shortfall of NK cells, he transfused the cells in frequent cycles that led many patients to have an adverse reaction from the constant influx of IL-2 into their bloodstream. Additionally, increasing the number of NK cells by 10 was insufficient. LAK therapy has also been used with a focus on increasing the numbers of Tcells however, as shown earlier, T-cells are of limited potency when it comes to fighting cancer.
In Japan, LAK therapy has been experimented with but until now, no doctor has been able to increase the number of NK cells efficiently. Teshigawara and Okubo have developed a therapy where they can increase the number of NK cells by over 1,000 times. Cells of patients at the clinic can be cultivated using the technology at Lymphocyte Bank—a general support service for ANK therapy.
Having studied the LAK process extensively, this pair of innovators saw that there were two key problems with existing treatments. Firstly, cells that had been taken out of the body were less powerful when they were returned, and secondly, it was difficult to increase the actual number of NK cells. After four years of study and research, started in 1991, they created a treatment by which they are able to take lymphocytes out of the blood—without causing problems resulting from blood loss—and increase the number of activated NK cells by up to 1,000 times. They call these cells Amplified Natural Killer (ANK) cells. The increased number of activated cells, when put back into the blood, not only provides a much greater volume of NK cells for the body to attack cancerous tumours, but also the activity of the cells draws a supportive response from NK cells that are dormant in cancer patients; this is based on the hypothesis that a major reason for the development of cancer in the first place is a deficiency in the body’s existent number of NK cells. In 2001, they were able to found the Higashi-no-touin clinic and Lymphocyte Bank to allow more patients to take advantage of the therapy.
Dr Teshigawara is confident about the suitable properties of NK cells: “NK cells move around the body in blood circulation and patrol for cancer cells. This makes the cells appropriate for dealing with any type of cancer and they perform the function of killing the cells with the greatest efficiency.” NK cells, unlike cytotoxic T-cells, do not require to be ‘taught’ to recognize cancer cells, they naturally find and destroy cancer cells.
To summarize, the success rate of ANK compared to that in the other two therapies in terms of the cells’ ability to kill cancer cells is significantly higher (see Figure A). Comparatively, T-LAK treatment is able to increase the number of T-cell lymphocytes but is lacking in strength. LAK treatment is able to strengthen NK cells but not increase the volume sufficiently. ANK treatment, on the other hand, increases the number of NK cells and these activated NK cells are much more successful in the destruction of cancer cells (see Figure B).
The treatment in practice
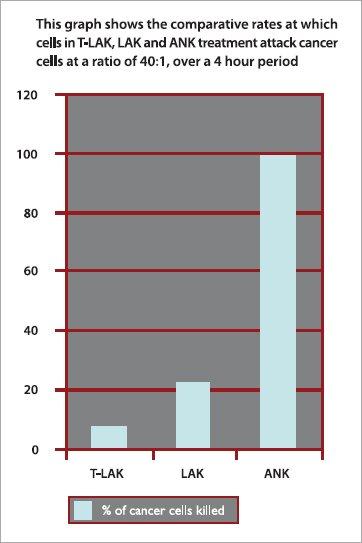 Figure A: ANK cells are much more successful at killing cancer cells
Figure A: ANK cells are much more successful at killing cancer cells
Teshigawara and Okubo argue that although increasing the number of NK cells is a crucial development, ANK therapy requires much more than just putting cells back into the body. They devote a large proportion of their time and resources to the customization of how many ANK cells are needed to kill or contain the cancer, and the frequency at which they are added: the key is to maintain the balance so that it is never in favor of the cancer. One course of treatment typically involves the transfer of ANK cells twice a week for a period of six weeks. However, Dr Okubo is quick to emphasise that every patient is a different case: “Each cancer requires careful management. We need to monitor the body’s response extensively and know what to look out for. We can tailor the treatment to each patient.”
Based on clinical trials, ANK therapy has had a good track record so far. When at the trial stages during its initial development at a famous national university, a patient—Mr Harada—was suffering from a severe lymphoma and became involved with the project in 1992. He had been given only eight months to live but ANK therapy was extremely effective and he is still alive today. In another instance, a Japanese male in his fifties was suffering from a malignant follicular tumour (B-cell type). The cancer was slow developing and had spread all over his body. This made surgical operation redundant and anticancer drugs had failed to improve his condition. In combination with antibody drugs, he underwent ANK therapy twice a week for a course of five weeks at the Higashi-no-touin clinic and his cancer went into remission. After five months the cancer had reduced by 50%, (see CT scan, right) and after a few more months the cancer went into complete remission.
When asked about the risks involved with this treatment, Teshigawara and Okubo state that in terms of side-effects there is little to worry about. There is the possibility of a chill or fever when activated cells are returned to the body but this is not severe. NK cells produce cytokines and this generates heat—when NK cells are multiplied at an increased rate there is a greater amount of cytokines, and therefore more heat, and this can lead to a fever. When ANK cells awake other passive NK cells, they leave the veins and this can cause a chill. However there are two more noteworthy drawbacks to the treatment.
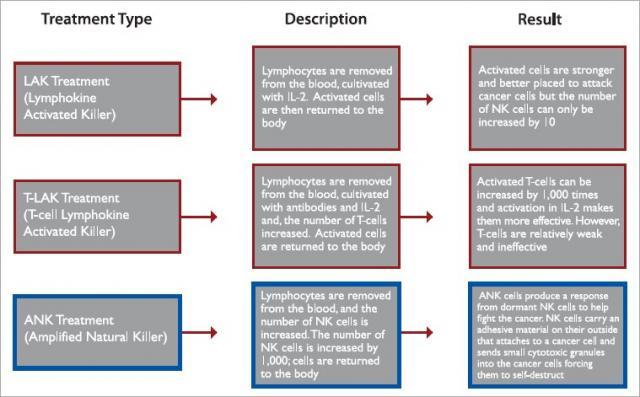 Figure B: Comparative analysis of LAK, T-LAK and ANK treatments
Figure B: Comparative analysis of LAK, T-LAK and ANK treatments
The cost
For one course of treatment the price is ¥4,000,000 (roughly US$35,000)
Impaired quality of NK cells
Most patients who have tried ANK treatment to date have previously undergone another treatment such as chemotherapy. This can impair the NK cells and thus hinder ANK treatment.
In order to address these issues, Teshigawara and Okubo, along with the technical support of Lymphocyte Bank, are certain that if they can overcome the second problem, the first will be solved; by making ANK therapy work to its maximum capability, the number of necessary courses of treatment can be reduced and thus cut down the cost. There are three solutions that can make ANK therapy more effective:
1. Combination with surgical oncology.
There is a good synergy with this treatment because if the major tumours can be removed, the ratio of ANK cells to cancer cells can be increased. In turn, ANK therapy can reduce the need for more traumatic surgery than is necessary, and, removal of tumours has no negative effect on the body’s NK cells.
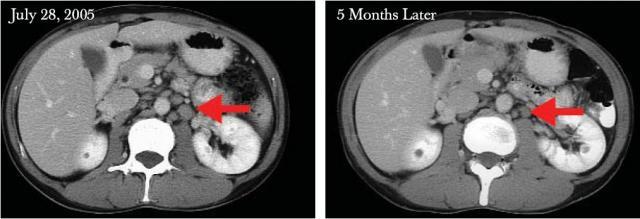 A malignant follicular lymph node tumour, reduced by 50% by the mid-stages of the treatment
A malignant follicular lymph node tumour, reduced by 50% by the mid-stages of the treatment
2. Combination with antibody drugs. There are so-called molecular targeting drugs available: they target a specific antigen and can successfully prevent cancer cells from multiplying. By containing the cancer in this way, ANK cells are much better placed to perform their termination function. Again, there is no negative effect on the body’s NK cells. Antibody drugs themselves alone would suppress growth of cancer but they don’t actually kill the cancers cells. What they do is to stimulate NK cells to find and kill cancer. The antibody drugs also coat cancer cells in antibodies that allow NK cells to recognize which cells they need to attack. They do so by releasing cytotoxic granules; an activity termed as Antibody Dependent Cell-mediated Cytotoxicity (ADCC).
3. Early incubation of lymphocytes. Although other treatments may be advisable, because of the negative effect on NK cells, Teshigawara and Okubo encourage patients to allow them to siphon off a good quantity of cells before they undergo other therapies. This gives them the healthiest cells possible to work with.
Uniting all these three solutions is the aim of allowing the ANK cells to perform to their maximum ability.
 Dr Teshigawara, architect of ANK therapy
Dr Teshigawara, architect of ANK therapy
Dr Okubo is frank about the complexities of the cultivation process he has developed and remarks that “it is difficult to understand. Before it can be used anywhere else in the world, doctors need to come here and study it. At the moment it exists only in Japan.” However, he is excited about ANK as it can be used to treat a range of different cancers including colon, prostate, lung, and mouth cancers. He recalls that there was even a Hepatitis C patient he was treating who also suffered from liver cancer—the ANK therapy successfully destroyed the cancer cells.
How does the process work?
For Teshigawara and Okubo, to be able to perform their treatment, initially, they like to see a patient, learn about their condition, and explain as much as they can about what they might be able to do with ANK treatment. Then, if the patient decides to proceed, they get the details of all therapies tried to date and make a plan for therapy.
Using Lymphocyte Bank technology, it takes four hours to isolate lymphocytes; the machine removes them from the circulation while allowing the rest of the blood to flow back into the body so that there are no problems from blood loss.
Isolated lymphocytes are cultivated and the number of NK cells is increased; this takes, on average, a period of two to three weeks. After this, lymphocytes are infused via a drip back into the patient’s body where they get to work, immediately fighting the disease. The therapy is under constant micromanagement and it is the time and technology involved that inflates the cost. However, for an initial consultation, there is no charge and a thorough assessment can be made before patients have to finally decide whether or not to proceed.
At present, this treatment is not well known and is available only in Japan. There are 15 hospitals in Japan that can perform ANK treatment in association with the Higashi-no-touin Clinic and the Lymphocyte Bank. Readers wishing to organize a free and fully confidential consultation can direct enquiries to the contact details below.JI
Contact details
Lymphocyte Bank
President: Fujii Masanori
Kyodo Building 1, 2F
1-5-5 Kudan Minami,
Chiyoda-ku, Tokyo
Tel: +81-3-3556-7380
Fax: +81-31-3556-7506
Email: sec@lymphocyte-bank.co.jp and cancertherapy@japaninc.com
Web: www.lymphocyte-bank.co.jp and www.cell-therapy.jp
J@pan Inc Magazine, Nov/Dec 2007






Comments
Anonymous (not verified)
December 6, 2007 - 01:41
Permalink
Nobel Prize Candidates
These doctors are to be congratulated for pionerering this new cancer therapy; has anyone nominated them for a Nobel Prize yet?
Appolonius (not verified)
October 3, 2008 - 07:25
Permalink
"New" Cancer Treatment
Sumimasen, Onarosan. There have been plenty of curative alternative cancer treatments available for some time; among them, pioneer work by Dr. Royal Rife as well as many others. Allopathic TREATMENTS cost a lot of money for little return to the patient and big return to the pharmaceutical companies. Though I imagine your world view cannot countenance that alternatives exist. Simply notice whether you find yourself in violent disagreement or in curiosity to explore the narrative outside of the box. Any vehement disagreement will indicate a psychic cathexis to a certain set of ideas about the nature of reality, in this case, modern allopathic "medicine". A true scientific method will always consider that current theory is simply the best explanation to date, pending further investigation. In other words, when the M.D. tells you your condition is incurable, he simply means to say that he knows no way to cure you. He will readily supply you with his conclusion, and rarely with the process through which he arrived at said conclusion. Unfortunately, as has been noted, nothing so advances the cause of science as the death of old scientists.